Kidneys are one of the main organs involved in the excretory system within the vertebrate kingdom. Their main function is to filter out excess toxins and tiny metabolic wastes from our bodies through the creation and excretion of urine. The kidneys are vital organs for sustaining life, with it being physically impossible to continue to function without them. Without access to a properly functioning renal system, all excess toxins and waste products created within our bodies would have no way out, allowing them to continue building up until our cells are eventually poisoned to death. Wee(!)
Many mammalian species are born with two kidneys, although it is possible to live with just a single one with next to no problems arising. In fact, most mammalian life (including humans) can be sustained with just a single kidney functioning at just 75% of its maximum capacity. In the absence of a second working kidney – either from birth or from gradual defect – a process known as hypertrophy can occur. This is where the single kidney left, along with all of its individual components, physically grow and adjust in order to produce and filter equal amounts of urine as two fully functioning kidneys. This does not by any means indicate that you should sell one of them off, though. (They’re buddies, don’t be a monster and separate them unnecessarily)
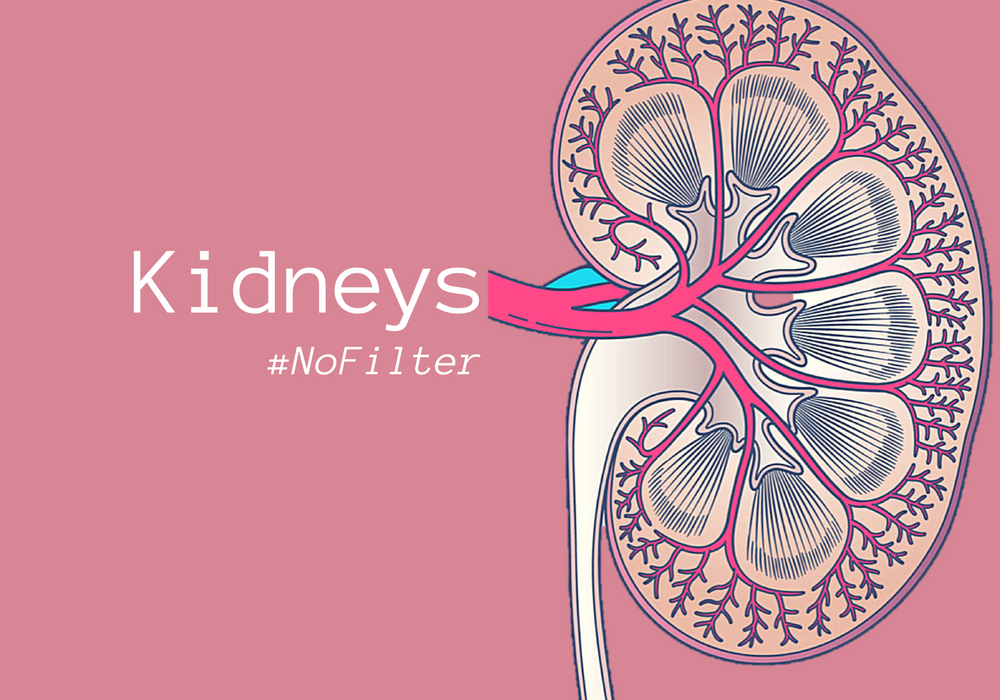
Each kidney is attached to a ureter – a duct, where the finished urine product drains into. The ureters feed into the urinary bladder, where your pool of pee is stored until it is squeezed out in a timely manner through our beloved urethra. Finally, our liquid toxin guests have made their exit, from their stay in Hotel: Human Body, down into destination: Toilet Bowl. Or, wherever it is that you decide to handle your business. The actual kidney itself is mainly distinguished by two sections: the outer cortex area and the medulla situated within. Spanning these two sections are our tiny, urinary heroes – the nephrons!

The nephrons are our main event, here at Pee-topia. The functional units of the kidneys, nephrons are microscopic tubules which filter out all of the toxins and waste from our blood plasma passing through the kidneys, converting it all into urine. Around 120 litres of fluid pass through the approximate million nephrons situated within a single kidney per day. (Make sure you drink up, folks.) Now, there are three key events leading up to the creation of urine: ultrafiltration, selective reabsorption and water reabsorption. Let’s take a trip down the kidney and find out how this all occurs.
Up in the cortex, the nephron starts at the glomerulus – the fancy word deemed appropriate for a bunch of squished up capillaries getting all friendly with each other. Being so condensed in a tight ball, with blood entering through the wide afferent arteriole and exiting through the narrower efferent arteriole, creates a high blood pressure within the glomerulus. This in turn, squeezes most of the fluids out from the blood plasma and deposits them into the Bowman’s capsule. This process is known as ultrafiltration. There are restrictions to this passage, however: large proteins and blood cells are unable to pass through the capillaries into the capsule. This is due to the podocytes (creepy, finger-like projections) lining the Bowman’s capsule, preventing large molecules from passing through (think of them as the Gandalf of the kidneys). The glomerular filtrate now sitting in the lumen of the outer capsule mainly consists of water, glucose, salt, inorganic ions, amino acids and urea from the liver. The remaining proteins and such in the blood plasma are then free to exit the glomerulus through the efferent arteriole. Most of the glomerular filtrate left in the Bowman’s capsule, however, is too precious to pee out. Onto the next part wee go!

Our body’s refusal to excrete the good stuff is known as selective reabsorption. Still in the cortex of the kidney, our star of the show is now the proximal convoluted tubule – also known as the PCT. All glucose, amino acids and vitamins from the glomerular filtrate are taken back into the bloodstream via the help of co-transporter proteins. Some salts (Na+ and Cl− ions) are also reabsorbed into the blood, as well as small quantities of water molecules via osmosis. In order for large doses of water to be reabsorbed, however, a counter-current exchange system (also known as the Hairpin counter-current multiplier) is in check.
Moving into the loop of Henle situated within the medulla of the kidney, the residual glomerular filtrate prepares itself to be transformed into concentrated urine. This is achieved via water reabsorption, aided by active Na+ and Cl− ionic pumps. The loop of Henle is divided into two major parts, consisting of an ascending and descending limb. The ascending limb is thicker in comparison to the descending limb and is also completely impermeable to water. Na+ and Cl− ions from the glomerular filtrate are actively pumped out of the ascending limb. This creates a steep osmotic gradient directly outside of the loop, causing water to diffuse out of the permeable membrane of the descending limb. As the filtrate moves down the loop of Henle, it becomes more concentrated due to this loss of water. However, whilst moving back up the loop, the filtrate yet again becomes diluted due to the diffusion gradient caused by Na+ and Cl− ions being actively pumped outside the ascending loop while maintaining whatever water is left (due to the osmotic-impermeable membrane). This is how the counter-current exchange system in constantly kept intact.
Our goal, however, is to keep more of that precious H2O inside of our bodies, rather than squeezing it all out. As the filtrate becomes more dilute at the top of the loop of Henle, water potential increases when moving into the distal convoluted tubule (DCT) and the collecting duct, thus allowing osmosis to take place and once again leave us with concentrated urine. Salt concentrations are also adjusted within the DCT, such as H+, K+, Na+ and Ca2+ ions, in order to regulate the pH of the resulting urine. Whatever is left of the filtrate – mostly urea, some water and light salt content – is then passed through the collecting duct and drained down the ureter and stored in the bladder, ready for excretion.
The amount of water reabsorbed in the collecting duct of the renal system is determined by the body’s current state – shifting between hydrated and dehydrated situations. This is controlled by anti-diuretic hormone (ADH). When concentrations of blood is high, this is detected by the pituitary gland in the hypothalamus, resulting in the secretion of ADH to alter the permeability of the collecting duct walls. Upon low water potential detected during dehydration, ADH is released in order to allow higher reabsorption rates of water back into the blood by making the collecting duct more permeable to water – thus creating more concentrated urine. Hydrated instances compose of the opposite, however, with higher water potential resulting in less ADH being released. This allows greater water retention within the collecting duct, ultimately resulting in more dilute urine in order to prevent overhydration. This is why the osmoregulation of the mammalian body is so crucial and heavily dependent on the kidneys being able to perform their job correctly. The hardest workers do it for free because they love you.
So, the overall conclusion: Are kidneys important? Just a wee bit. Look after your beans! We hope you enjoyed learning about the science behind peeing. Follow our blog and our Twitter/Instagram to make sure urine the loop!



Blog update – In The Mind Library
[…] Kidneys – No beans, just urine (#NoFilter) […]
DIY Detox: your body’s response to toxins – Seeking Science
[…] help detoxify our bodies by creating urea and filtering it out of the body via urine (more on that here). Most of all though, the hero of all detoxifying processes comes down to the one individual: the […]
Making a splash: an introduction to schistosomiasis – Seeking Science
[…] growth projecting from a mucous membrane), glomerulonephritis (inflammation of the glomeruli of the kidneys), as well as the symptoms mentioned […]