Madeeha Hoque

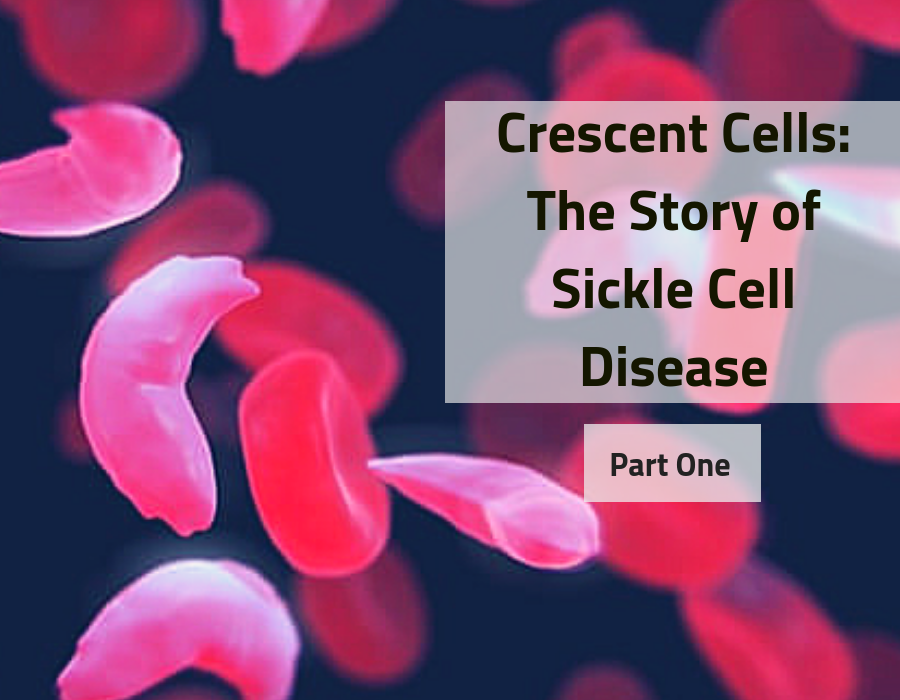
Our first post in our new Genetic Diseases series has arrived! Today we will be delving deep into the course of the blood stream – that’s right, we’re tackling Sickle Cell Disease.
Sickle cell disease (SCD) is a group of genetically inherited disorders that affect haemoglobin. Haemoglobin is the protein in our red blood cells (also known as erythrocytes) that delivers oxygen around our bodies – including all of our vital organs and muscles, in order to help them function smoothly. The disease mainly affects people of African, Asian, Caribbean, Mediterranean and Middle Eastern descent, being found more commonly in African or Caribbean family backgrounds. It is the most common inherited blood disorder in the USA, affecting approximately 80,000 Americans, with an estimated 1 in 500 African Americans and 1 in 1,000-1,400 Hispanic Americans being affected. The most common type of sickle cell disease is known as sickle cell anaemia (SCA), which is the most well-known disorder out of the sickle cell disease group. SCD causes a lot of lifelong problems which make it difficult to live a healthy life, but we will get onto all of that later. For now, let’s take a look at the causes.
As mentioned above, this debilitating disease is genetically inherited, with symptoms often beginning to appear from an early age. It is caused by a mutation in the autosomal recessive HBB gene, which, if present in both parents, has a 25% chance of being passed on to offspring. In order to understand how this mutation develops, however, we must first understand how haemoglobin works.
Haemoglobin is a metalloprotein contained within most red blood cells of almost all vertebrates, using iron molecules to transport oxygen around the body to the lungs or gills of the organism. Haemoglobin has a structure consisting of four globular protein subunits, typically with two subunits each of alpha-globin and beta-globin. The HBB gene codes for instructions on the creation of beta-globin, therefore, a mutation in this gene leads to either low levels of beta-globin (known as beta thalassemia) or abnormal beta-globin subunits being formed. A particularly common abnormal version of beta-globin is known as haemoglobin S (HbS), with other known abnormalities being known as haemoglobin C (HbC) and haemoglobin E (HbE) subunits.

People suffering from sickle cell disease, more commonly than not, have at least one of their normal beta-globin subunits replaced with haemoglobin S. The second beta-globin subunit is replaced by another of the abnormal subunits mentioned above. For example, those suffering from sickle-haemoglobin C (HbSC) disease tend to have haemoglobin molecules containing the haemoglobin S and haemoglobin C subunits instead of two normal beta-globin subunits. It is possible for different mutations to occur simultaneously also, where haemoglobin S is produced as well as beta thalassemia occurring. This disease is known as haemoglobin S-beta thalassemia (HbSBetaThal) disease and is incredibly rare and fatal if present. The most common form of SCD found, however, is sickle cell anaemia – a result of a mutation of the HBB gene causing both beta-subunits in haemoglobin to be replaced by haemoglobin S.

The abnormality of these different versions of beta-globin subunits distorts the red blood cells and causes them to form a more rigid, crescent-like sickle shape, as oppose to their regular, biconcave disc form. This abnormal shape causes premature death of red blood cells, which eventually leads to anaemia, due to the lack of red blood cells readily available. Since oxygen has an affinity for the iron atoms which are present within the haemoglobin molecules found inside of red blood cells, less oxygenated blood is pumped throughout the body to the organs. This is due to the inevitable lack of red blood cells being present to carry the oxygen to them – thus causing anaemia. Not only this, because of the distortion of the shapes of these abnormal erythrocytes, these red blood cells can get stuck in blood vessels due to their inflexible sickle-shape, causing many medical complications to occur – such as high blood pressure.
Next time, we’ll delve further into the symptoms of SCD, and potential treatments for the disorder – don’t forget to follow us on Twitter and Instagram to be notified when Part 2 is published!


Crescent Cells: The Story of Sickle Cell Disease (Part Two) – Seeking Science
[…] week’s post with the symptoms, diagnostics and management of Sickle Cell Disease (SCD). Click here for a quick peek at our previous post, introducing sickle cell […]